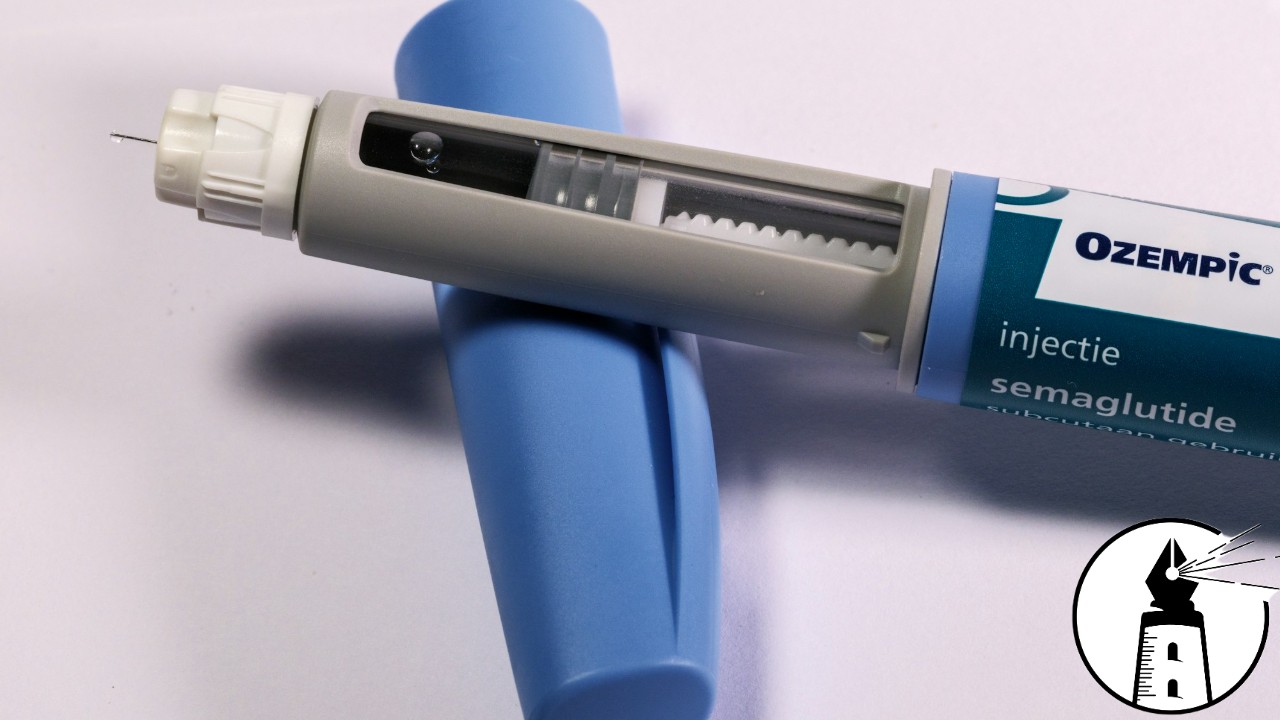
New research presented at a major endocrinology conference has added another layer of complexity to the growing demand for popular weight loss medications like Ozempic and Mounjaro. These drugs, originally developed to treat Type 2 diabetes, have become widely used for weight management. Now, new findings suggest they may also help restore testosterone levels in men with obesity or diabetes.
Testosterone levels in men typically begin to decline in the late 30s or early 40s. By age 75, the average level drops to about 65 percent of what is seen in young adulthood. When testosterone falls below a certain threshold, it can contribute to serious health issues. Low levels have been linked to decreased bone density, reduced muscle mass, diminished libido, and lower red blood cell counts.
In this recent study, researchers reviewed medical records from men who had been prescribed GLP-1 receptor agonists such as Ozempic and Mounjaro. They tracked testosterone levels before and during 18 months of treatment. The majority of men who started out with low or borderline levels eventually reached a normal range without the need for testosterone replacement therapy. These changes were attributed to improvements in metabolic health and weight loss, which allowed the body’s natural hormone production to rebound.
This finding has implications for men who are already undergoing testosterone therapy. If levels return to normal on medications like Ozempic or Mounjaro, some may need to reduce or even discontinue their supplements. There is increasing concern within the medical community about the overuse of testosterone therapy, particularly in men with low-normal levels and no identifiable medical cause. Direct-to-consumer advertising has played a role in driving this demand, often blurring the lines between clinical necessity and lifestyle enhancement.
Women were not included in this study, as the same testosterone-boosting effect was not expected. In women, testosterone is typically only measured when symptoms of hormonal imbalance are present, such as irregular menstrual cycles, excessive facial hair, or signs of masculinization. In women with conditions like polycystic ovary syndrome, GLP-1 medications have shown potential to slightly reduce elevated testosterone levels by improving metabolic function.
As more men turn to Ozempic and Mounjaro not just for weight loss but also for perceived hormonal rejuvenation, access to these medications could become even more difficult for patients with diabetes or severe obesity. This situation mirrors what happened with Viagra, which was originally developed to treat heart disease but became widely known for its unintended effect on sexual function. What was once a targeted treatment became a mass-market commodity.
If Ozempic and Mounjaro continue down the same path, they may soon be in high demand among men experiencing a midlife crisis, further competing with those who need these drugs for life-threatening medical reasons. Rising demand from wealthier individuals and off-label use could strain supply chains, increase costs, and leave vulnerable patients waiting for medications that were originally meant to manage chronic illness.
Once Ozempic becomes available in generic form, it is likely to follow the same marketing trajectory as other overprescribed medications. Late-night television and podcast sponsorships will flood the airwaves with less than tasteful branding, repackaging a serious treatment as a lifestyle shortcut. As interest in these medications continues to expand, healthcare providers and regulators face a growing challenge. Ensuring that access remains fair and medically justified will be essential to prevent another case of pharmaceutical drift from necessity to vanity.
—By Greg Collier